Breast Implants, Breast Cancer and Screening
)
There are controversial and contradictory information about breast implants, breast cancer and breast cancer screening. There is the concern that breast implants can cause cancer, or that it affects the detection of cancer, including the effectiveness of screening mammograms. There are numerous studies and reviews conducted over the years, and several conclusions can be drawn:
1. Augmentation patient are not at a greater risk of developing breast cancer.
This concern came out of studies in rats back in the 1940's where foreign objects implanted in them increased their risk of developing sarcomas. However, this was never found to be the case in humans, in fact, several studies have both refuted this fact and also found no association between breast implants and breast cancer.
However, breast implant associated anaplastic large cell lymphoma (BIA-ALCL) and breast-implant associated squamous cell carcinoma have recently been in the spotlight and is definitely a condition associated with breast implants as the name suggests. This is, however, NOT breast cancer. To find out more about BIA-ALCL and BIA-SCC, read about it on our 'All About Implants' page.
2. Early detection of breast cancer is possible in patients with breast implants.
There have been several studies in that showed there was no difference in the severity or stage of breast cancer between implant and non-implant women. Breast cancer can still be detected while in its early stages in patients with breast implants.
3. Breast cancer is not more aggressive in patients with breast implants.
The studies have shown that the type of breast cancers are the same between the two groups, and the survival rates are also similar.
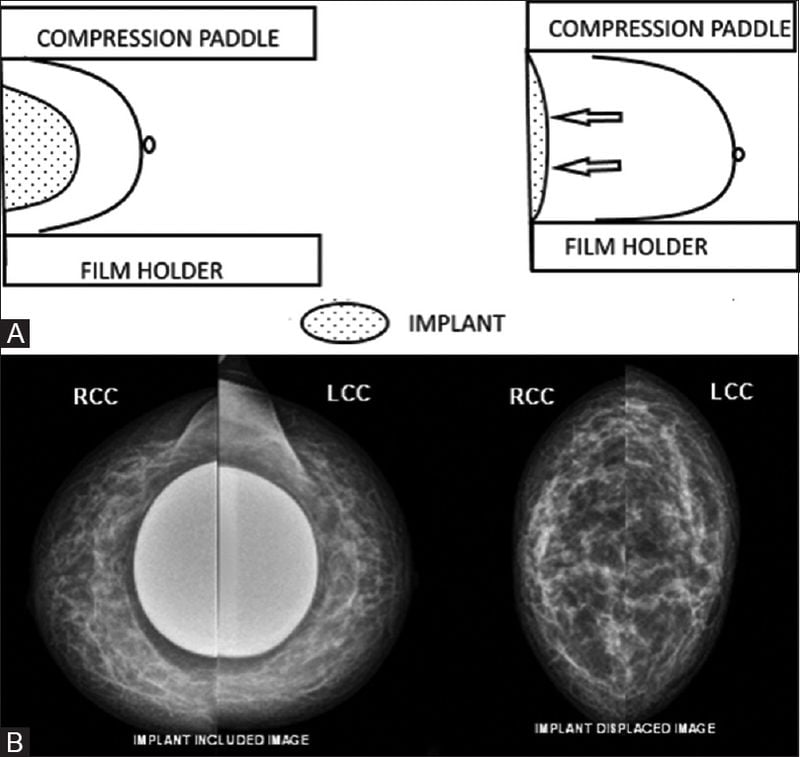
4. Eklund views should be used when obtaining mammograms in patients with breast implants.
The sensitivity for standard mammography has been questioned in patients with breast implants because the implants (both saline and silicone) can interfere with the ability to visualise breast tissue and adequate diagnosis. It was found that up to 85-90% of the breast tissue can be obscured by the implant during a standard mammography. However, a technique was developed in 1988 by Eklund in which the implant is displaced posteriorly during the mammogram to allow visualisation of 85% of the breast tissue, regardless of implant shape or size.
5. Submuscular (under the muscle) placement of implants allows for better visualisation in mammograms.
In general, studies have shown that even with Eklund views, the submuscular (under the muscle) implant allows for greater visualisation when compared to the subglandular (over the muscle) implant.
6. Silicone and saline implants looks the same on mammograms and neither is better to the other in screening.
Both Silicone and saline implants compresses the breast tissue the same, thus neither is better in mammography.
7. Alternative modalities have their own limitations.
Alternative modalities have been suggested, such as ultrasounds and Magnetic Resonance Imaging (MRI) to increase sensitivity in detection of breast cancers in patients with breast implants, especially in patient who are concerned about implant rupture from a mammogram. Alternative imaging methods may also be necessary if there is already implant rupture or evidence of capsular contracture, as these are some of the relative contraindications for routine mammograms.
Although ultrasounds can be helpful for diagnosis of implant rupture and capsular contracture, it cannot detect microcalcifications, thus it is not an ideal screening tool for breast cancer. This test is also highly operator dependent as it relies heavily on the ultrasonographer to cover all of the breast tissue during their scan.
MRI can fully visualise breast tissue, but intravenous contrast is often necessary. Although its sensitivity is over 90 percent, its limitation lies in its lower specificity, with increase false positives, where benign conditions of the breast may appear to be malignant tumours, resulting in over-diagnosis and unnecessary tests. Breast MRI is currently non-rebatable (with Medicare) for individuals with no immediate family history or personal history of breast cancer.
8. The current recommendations for screening mammograms are no different for patients with implants (compared to the normal population).
The current recommendation is that women between the ages of 45 and 70 should have a mammogram every 2 years. These recommendations hold for both women with or without breast implants. The recommendation is different for those with family history, previous breast cancer and those with higher risk factors. Please consult your doctor to find out when and how often you should be having your breast screening and the best modalities for your screening program.
) Author:Dr Lily Vrtik
Author:Dr Lily Vrtik| Tags:plastic surgeryBreast implantsBreast |